WHAT IS IN THE TREASURE HUNT BOX?
What do Treasure Hunts have to do with maths you ask? Maps and co-ordinates are a fun part of maths! The Explore magazine teaches kids how to read a map (including what a compass rose is and how to read a legend). They then get to have a go at making their own!
Kiwi Crate’s Treasure Hunt box comes with materials for three crafts:
DESIGN AND MAKE A TREASURE CHEST
Clear instructions and no wood glue required made this a delightfully age appropriate build! The treasure chest is not only nicely on theme for the topic but has also proved popular since for open-ended play. I will note that we had no success picking the lock so decided to set it aside before the keys inevitably got lost.
DESIGN AND EMBOSS GOLDEN COINS
Every treasure chest needs treasure! This was a fun open-choice activity that allows kids to design each face of three coins. There are a range of numbers and kiwis provided. Kids place their choices on the coins, add a golden sticker, and carefully smooth them until the bas-relief is visible.
MAKE YOUR OWN TREASURE MAP
There are lots of different paper options provided for making your own maps. a good place to start is to map a room / house / garden and see if someone can find where the treasure chest has been hidden. Another good map to make is how to walk or drive to some place that you go often like school, a park, or a library.
More Mapping Activities
National Geographic have lots of mapping activities that can be done at home! They provide the teaching ideas, images, and PDFs that can be downloaded. Check out:
- Exploring Maps and Models of Earth
- Land, Water, and Animals on a Map
- The Sun, Earth, and Cardinal Directions
- Cardinal Directions and Maps
- Reading a Resource Map
We are Teachers have lots of hands-on ideas with photographic inspiration: check them out here.
Some fun boardgames that teach reading grid co-ordinates include Peaceable Kingdom’s Race to the Treasure and the classic game Battleships.
HOW DO I ORDER KIWI CRATE?
This is not a paid review. I spent a lot of time searching the internet to find out more information about the Kiwi Crate and Atlas Crate boxes before deciding to try them and found the blog posts / photos that people shared were really useful!
If you would like to try Kiwi Crate (or one of their other lines), you can receive 50% off your first box by clicking here.
What I like about the Kiwi Crate kits is that they use a combination of Science, Technology, Engineering, Arts, and Mathematics to explore a concept or idea. There’s no obligation to sign-up in an on-going capacity so it’s easy to tie them in with birthdays / Christmas; the boxes are quite compact so they also store easily in a cupboard for bringing them out on a rainy day. Mind you, this only works if you spot the package on the door-step first – children become quite adept at recognising the green Kiwi Crate box and screaming with delight at it’s arrival!
The boxes are sent randomly so there’s no way to know what will come in the future; however, you can log-in to your account at the start of each month to see what box has been selected. Your box history is kept which means that even if you cancel and then pick-up again the following year they can make sure that you aren’t sent repeats of boxes.
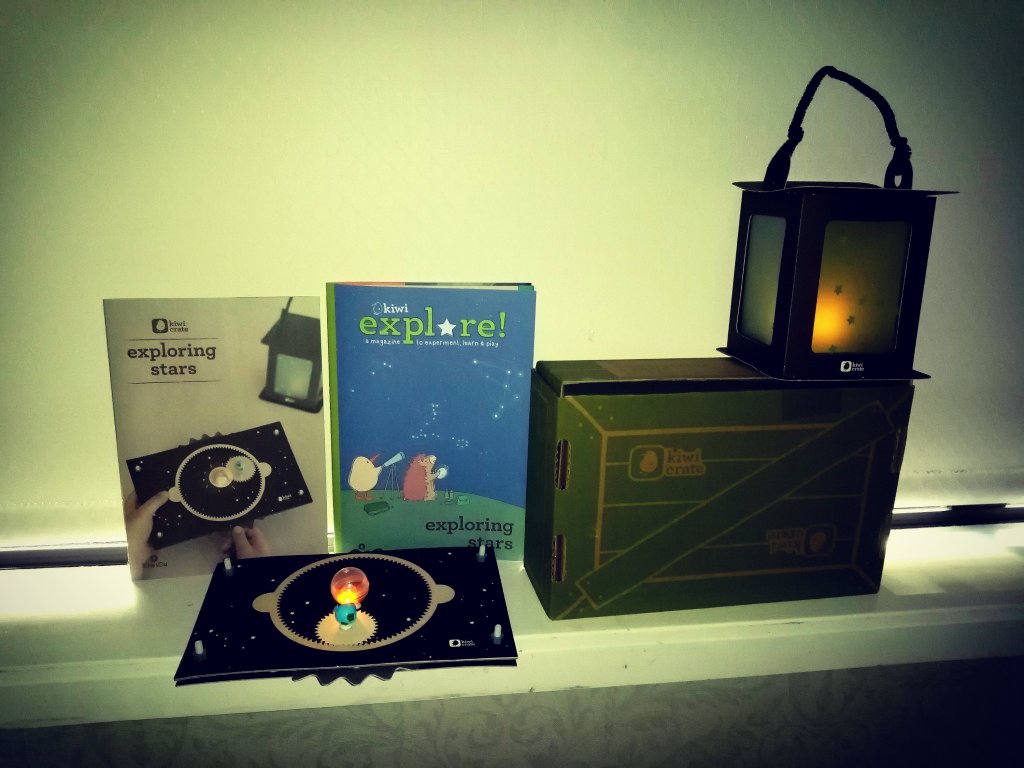
WHAT IS IN A KIWI CRATE?
The Kiwi Crate is aimed at ages 5-8 years. It comes with a copy of the Explore magazine which opens with a fun comic about Steve the Kiwi and his friends. [As a side note, these are made by an American company despite the use of our New Zealand native bird]. These comics are really approachable for younger kids and a great way of exploring the concepts being introduced in a relateable manner.
The Explore magazine provides a range of information on the topic, it might include some simple games or tricks to try at home, and provide ideas for additional crafts / activities using simple materials. It also has a sticker [unique to each box theme] to put on your Kiwi Crate chart.
The box also includes an instruction manual and the materials that you need to build the main craft. Generally, there are two activities to do – one that is more art related, and one that is more mechanical engineering. What makes the kits special, is how well crafted the engineering components are. They really are designed for the intended age group so that they can either build themselves or help assist an adult. There are handy visual images and checkpoints to make sure that things are aligned correctly. There is no super-bonding-fingers-together wood glue to use with these projects (which makes them great for highly sensory children); instead parts come with double sided tape finely engineered on so that you just need to remove the backing strip of paper.
Interested in more homeschool box reviews?
Discover the World with ATLAS Crate
Explore STEM with Kiwi Crate
#2 The Amazing Animation Box (make your own 19th century movie with a Zoetrope!)
#3 The Mechanical Sweeper Box (make your own baleen whale!)
#4 The Disc Launchers Box (play games with physics!)